1 dead, 101 in hospital: Behind Pune’s outbreak of Guillain-Barre syndrome
The number of suspected cases of this neurological condition reported from the region has crossed 101. Why is it happening and what can be done?

On Sunday, 26 January, as the nation celebrated Republic Day, the caseload of suspected Guillain-Barre syndrome (GBS) patients in and around Pune — which has been seeing an outbreak — inched past 100. And a patient in Solapur suspected of having contracted it while in Pune died. He was visiting his native village in Solapur at the time.
Of the 101 patients still under treatment across the region, 16 are on ventilator support.
The outbreak had already affected 73 people by the time the alarm was raised three days ago.
A visit by a team from the central health ministry is anticipated today, 27 January, to assess the situation. Meanwhile, the state has already ordered chemical and biological analysis of water samples from different parts of Pune, fearing contamination (see 'What is Guillain-Barre syndrome?' below).
Blood samples from the initial few days sent to the ICMR-National Institute of Virology have tested negative for chikungunya, dengue and zika. However, stool samples of nine patients tested positive for norovirus (a particularly virulent GI infection, more common in children) and three for Campylobacter jejuni (another GI infection — and a common predictor of GBS — which is often acquired via contaminated food and water).
Of the 101 suspected cases, the majority (81) are in the core area under the Pune Municipal Corporation, followed by 14 from the Pimpri Chinchwad Municipal Corporation’s space and another 6 from other districts.
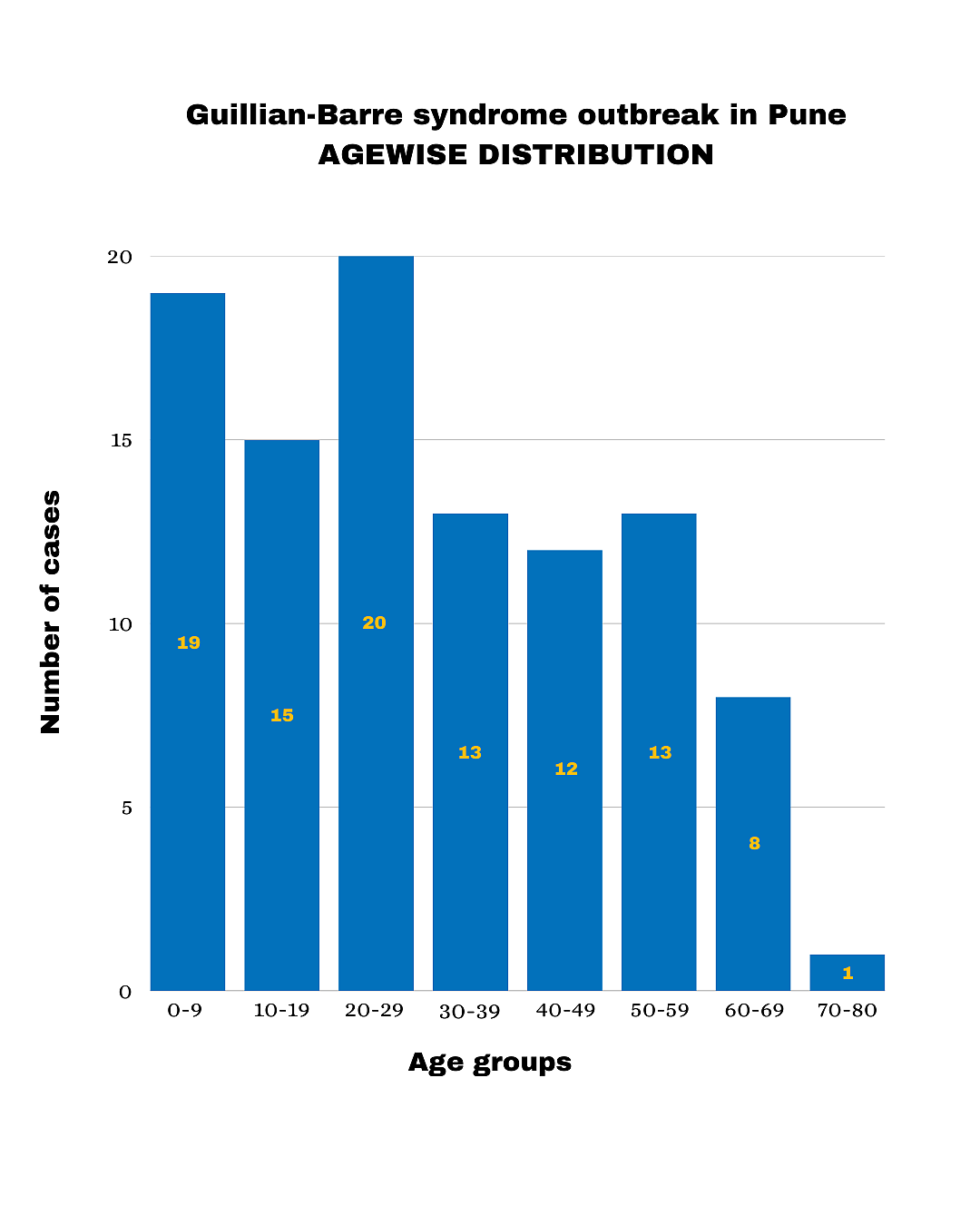
The current outbreak seems to have struck more than twice as many males as females (68:33) and the agewise distribution suggests more young people are being affected. This may be significant in helping healthcare professionals trace the outbreak to its root(s) since GBS is typically more common in the 50-plus age group.
The Hindu reported that the patient who passed away yesterday was first admitted to the hospital on 18 January with symptoms of respiratory illness (cough, breathing difficulties). And indeed, having started in the ICU, had seemed to be healing well, having been shifted to a regular room — until he deteriorated again and symptoms of paralysis were observed in the lower limbs.
He was then shifted back into the ICU, where he passed away from increased breathing problems.
What is Guillain-Barre syndrome?
GBS is a neurological condition that appears after certain severe infections, where the triggered immune system overreacts and starts stripping off the protective myelin sheath (the outermost fatty layer) of the long peripheral nerves. This causes numbness and paralysis starting with the limbs, because without that insulating layer, the nerves can no longer effectively relay electrical impulses to and from the brain.
It is more often triggered by GI and respiratory infections, both bacterial (one of the common ones being Campylobacter) and viral, including influenza, Covid-19 and zika (but it is also less common for it to occur from dengue, so not all viruses are implicated).
It does not commonly occur as a consequence of parasitic diseases such as malaria. However, it is also one of the rare side effects of attenuated or dead viruses in some vaccines.
There was, for instance, concern around the AstraZeneca Covid-19 vaccine showing a higher rate of it than other vaccines against the coronavirus during the recent pandemic. However, that vaccine was being phased out already, since more effective ones covering newer strains had already been put out which don't carry a similar risk (the ones using an adenovirus vector carry about a 2.4 times risk than the Covid virus itself, but the risk is 7 times lower with the new mRNA-based vaccines).
The swine flu (influenza) vaccine of 1976 was another implicated in some cases of GBS (1 extra case in every 100,000 people vaccinated), but it remains true that the vaccines in question are still considered ‘safe’ in all of these cases — simply because the rate of GBS associated with them is found to be less than that associated with getting the disease itself.
Or, in other words, reduced vaccination rates would not reduce the risk of GBS but would increase it instead.
Symptoms of GBS:
tingling that typically starts in the legs and progresses to weakness and numbness, eventually paralysis if not arrested;
difficulty walking, loss of balance and coordination;
difficulty speaking or eating (once the facial and oral nerves are affected);
breathing problems (once nerves to the torso are affected);
blurred vision or inability to move the eyeballs in different directions.
Precautions:
GBS is not itself contagious, though the diseases preceding it often are. The only real precautions for GBS are therefore to avoid the most commonly associated infections, and infections in general, since it is post-infection autoimmune syndrome.
This may mean:
using adequate insect repellents,
sticking to verified safe drinking water or drinking boiled water only,
avoiding cross-contamination between raw and cooked foods (it may be best to avoid raw foods when there is a community outbreak of GI diseases),
not eating using shared plates and utensils communally and not sharing towels while an outbreak is in progress,
observing good hand hygiene throughout the day and not just around meals,
avoiding touching your face (nose, mouth, eyes especially) as much as possible.
Getting vaccinated against vaccine-preventable diseases (VPDs) is part of it as well, since it lowers the risk, if not eliminating it entirely.
Treatment and recovery:
Most patients do recover fully from GBS within 2–4 weeks of onset of symptoms. However, some may be left with permanent nerve damage.
For those in whom ability to walk and eat etc. have been affected, recovery may take longer, depending on the severity, from months to as much as several years.
Treatment mainly consists of managing symptoms, as there is no known cure for the condition.
The fatality rate for GBS ranges from 3 per cent to 13 per cent globally, with the rate in India being 8.9 per cent (that implies 1 in 10 patients may die).
The last big outbreak of GBS to catch worldwide attention was in Peru in June 2023, when the nation put out an epidemiological alert with 231 cases over 28 weeks — a far lower rate than we are seeing in Pune, concerningly.
However, Peru also had a far more severe outbreak in 2019 — before the Covid pandemic — and that saw Campylobacter jejuni triggering almost 700 cases. The 2023 outbreak also saw a large percentage of Campylobacter infections.
Follow us on: Facebook, Twitter, Google News, Instagram
Join our official telegram channel (@nationalherald) and stay updated with the latest headlines
